What is osteoarthritis (OA)?
The most typical type of arthritis is osteoarthritis (OA). Degenerative joint disease or “wear and tear” arthritis are two names for it. It usually affects the hands, hips, and knees.
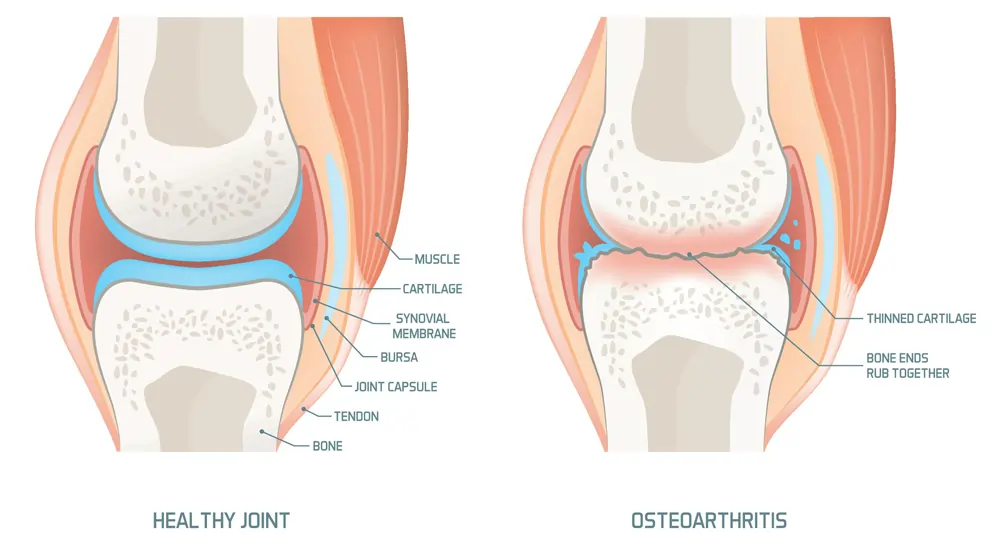
With osteoarthritis, a joint’s cartilage starts to degrade and the underlying bone starts to alter. These alterations typically take time to manifest and worsen. osteoarthritis may result in discomfort, stiffness, and edema. Some people lose the capacity to perform everyday duties or job because of it, which can also result in impaired function and disability.
What are the signs and symptoms of osteoarthritis?
- Pain or aching
- Stiffness
- Decreased range of motion (or flexibility)
- Swelling
How widespread is osteoarthritis?
Almost 32.5 million American people suffer with osteoarthritis.
What causes osteoarthritis?
The cartilage between the bones in the joints is harmed or breaks down, leading to osteoarthritis.
What are the risk factors for osteoarthritis?
- Overuse or injury to a joint can damage a joint and raise the risk of OA in that joint. Examples include knee bending and repetitive stress on a joint.
- Age—Age raises the risk of acquiring OA.
- Gender: Women are more prone than males to acquire OA, particularly after the age of 50.
- Obesity—Extra weight puts extra strain on joints, especially on those that support weight, such as the hips and knees. The risk of OA in that joint rises as a result of this stress. Moreover, obesity may have metabolic consequences that raise the risk of OA.
- Genetics: Individuals who have OA in their family are more likely to develop the disease themselves. Knee OA is more prone to develop in people with hand OA.
- racial factors— Certain Asian populations have a lower incidence of OA.
How is osteoarthritis diagnosed?
With a study of the symptoms, a physical examination, X-rays, and lab tests, a doctor can determine if you have osteoarthritis.
If there are any concerns about the diagnosis, a rheumatologist, a physician who focuses on arthritis and other associated disorders, might be of assistance.
How is osteoarthritis treated?
Since there is no known cure for osteoarthritis, doctors typically use a variety of therapy to address its symptoms, which may include the following:
- an increase in exercise
- physical treatment that incorporates workouts to build muscle
- Loss of weight
- Medicines, such as over-the-counter painkillers and prescription medications
- assistance tools like crutches or canes
- Surgery (if other treatment options have not been effective) (if other treatment options have not been effective)
In addition to these treatments, people can develop self-management skills to control their OA. People with osteoarthritis can engage in the activities that are essential to them thanks to these measures, which assist to lessen their pain and incapacity. These five quick and easy methods for managing arthritis can be useful.
How can I better my quality of life while managing osteoarthritis?
Five self-management techniques are advised by the CDC’s Arthritis Program for treating arthritis and related symptoms.
- Learn how to govern oneself. Attend a self-management education session to learn how to better manage your symptoms and your quality of life. Self-management education classes are beneficial for persons with OA, arthritis, and other chronic disorders. Learn more about the self-management education programs that the CDC recommends.
- Take up some exercise. Adults should engage in 150 minutes each week of at least moderate physical activity, according to experts. Every minute counts, and even a little activity is preferable to none. Walking, swimming, or biking are suggested as moderate, low-impact activities. Also, regular exercise helps lower the risk of developing other chronic conditions like diabetes, heart disease, and stroke. Find out more about the benefits of exercise for arthritis.
- Visit programs that encourage physical activity. Participation in physical activity programs can help reduce pain and disability caused by arthritis, improve mood and mobility for persons who are concerned that physical activity may exacerbate OA or are unaware how to exercise properly. Courses are held in the Ys, parks, and community centers in the area. Those with OA may feel better after taking these lessons. Learn more about the physical activity programs that the CDC recommends.
- Consult your physician. By keeping regular checkups with your doctor and according to their prescribed treatment plan, you can actively participate in managing your arthritis. If you also suffer from other chronic illnesses like diabetes or heart disease, then this is very crucial.
- Become thinner. Losing weight eases pressure on joints, especially weight-bearing joints like the hips and knees, in overweight or obese people. Achieving or maintaining a healthy weight can help with pain relief, function enhancement, and OA progression.
- Keep your joints safe. Arthritis can be aggravated or caused by joint injury. Pick arthritic-friendly exercises like swimming, biking, and walking. These low-impact exercises pose little danger of harm and do not twist or strain the joints. Find out more about safe exercising for people with arthritis.
Learn how to govern oneself. Attend a self-management education session to learn how to better manage your symptoms and your quality of life. Self-management education classes are beneficial for persons with osteoarthritis, arthritis, and other chronic disorders. Learn more about the self-management education programs that the CDC recommends.