Shoulder joint replacement, also known as Shoulder Arthroplasty (SA), is a surgical procedure aimed at reducing pain and restoring mobility in patients who have reached the final stage of shoulder arthritis or have suffered a severe shoulder fracture. This surgery not only alleviates pain but also helps in restoring movement, strength, and function of the shoulder.

- Surgery Statistics and Outcomes
- How Shoulder Joint Replacement Surgery is Performed
- Shoulder Arthritis: Causes and Complications
- Reasons for Treating with Shoulder Joint Replacement Surgery
- Signs Indicating the Need for Shoulder Joint Replacement
- Diagnosing Conditions Treatable with Shoulder Joint Replacement
- Ineligibility Criteria for Shoulder Joint Replacement
- Alternative Approaches Before Deciding on Surgery
- The Process of Shoulder Joint Replacement Surgery
- Types of Anesthesia in Shoulder Joint Replacement Surgery
- Stages of Traditional Shoulder Joint Replacement Surgery
- Reverse Shoulder Joint Replacement
- Types of Shoulder Joint Replacement Implants
- Risks and Complications of Shoulder Joint Replacement
- Recovery Time After Shoulder Joint Replacement Surgery
- Cost of Shoulder Joint Replacement
Surgery Statistics and Outcomes
Research indicates that approximately 95% of patients experience pain-free shoulder function one year after the surgery. This allows them to perform specific shoulder exercises to regain strength and movement. Many of these patients can return to their favorite physical activities such as golf, tennis, swimming, yoga, or Pilates, which they previously avoided due to shoulder pain.
How Shoulder Joint Replacement Surgery is Performed
Shoulder joint replacement, also known as Total Shoulder Arthroplasty, involves removing parts of the shoulder joint and replacing them with artificial prostheses. This is done to reduce pain and restore the range of rotation and movement of the shoulder. This surgery is highly successful in treating severe pain and stiffness caused by the final stage of arthritis.
Shoulder Arthritis: Causes and Complications
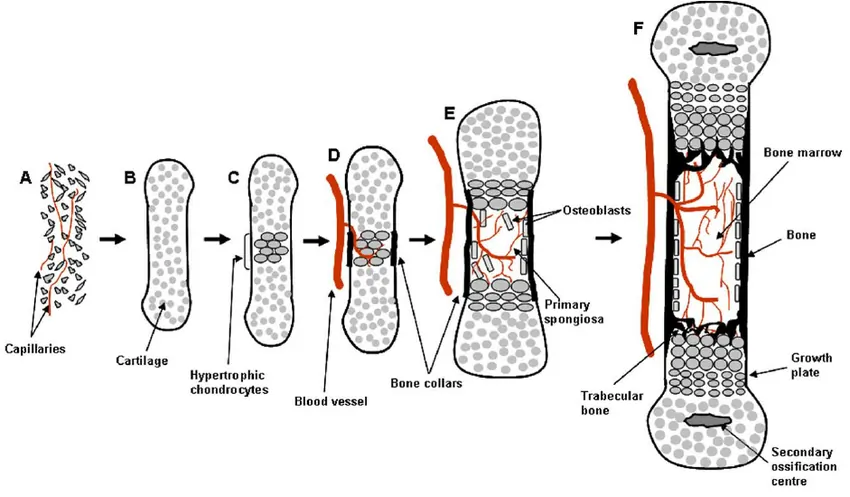
Shoulder arthritis is a condition where the soft cartilage covering the shoulder bones wears away or disintegrates. In a healthy shoulder, this cartilage allows bones to smoothly glide against each other. Without these cartilage surfaces, bones come into direct contact, increasing friction and causing damage to each other. Bone-on-bone contact can be extremely painful and difficult. Replacing these surfaces through surgery with artificial implants restores pain-free movement, strength, and function.
Reasons for Treating with Shoulder Joint Replacement Surgery
Shoulder joint replacement surgery is used to treat various problems affecting the shoulder. The two main types of arthritis that impact the shoulder are:
- Osteoarthritis (OA): This type of arthritis occurs due to wear and tear of the cartilage within the joint, mainly seen in older individuals or athletes who put constant pressure on their shoulders. It can follow injuries such as rotator cuff tears or shoulder fractures.
- Inflammatory Arthritis (IA): This term refers to a set of autoimmune diseases that directly affect the shoulder, like rheumatoid arthritis and ankylosing spondylitis. In many cases, shoulder joint replacement surgery helps in reducing pain and improving shoulder function.
Signs Indicating the Need for Shoulder Joint Replacement
To determine the need for shoulder joint replacement, it is important to pay attention to signs such as persistent arthritis pain not manageable with non-surgical treatments. Progressive stiffness and the feeling of grinding in the shoulder can also indicate this need.
Diagnosing Conditions Treatable with Shoulder Joint Replacement
For diagnosing shoulder arthritis, doctors typically use X-rays, CT scans, and Magnetic Resonance Imaging (MRI). These imaging tests are crucial for assessing the condition of bones and soft tissues around the shoulder. Additionally, if nerve damage is suspected, EMG tests or nerve conduction studies may be conducted to examine the nerves supplying the shoulder muscles.
Ineligibility Criteria for Shoulder Joint Replacement
Shoulder joint replacement is not suitable for all patients. Some patient groups who are not ideal candidates for this surgery include:
- Patients without significant debilitating symptoms
- Individuals whose rotator cuff and deltoid muscles are paralyzed
- Patients with active infections
- People with progressive neurological diseases affecting the joint (these cases are assessed individually)
Alternative Approaches Before Deciding on Surgery
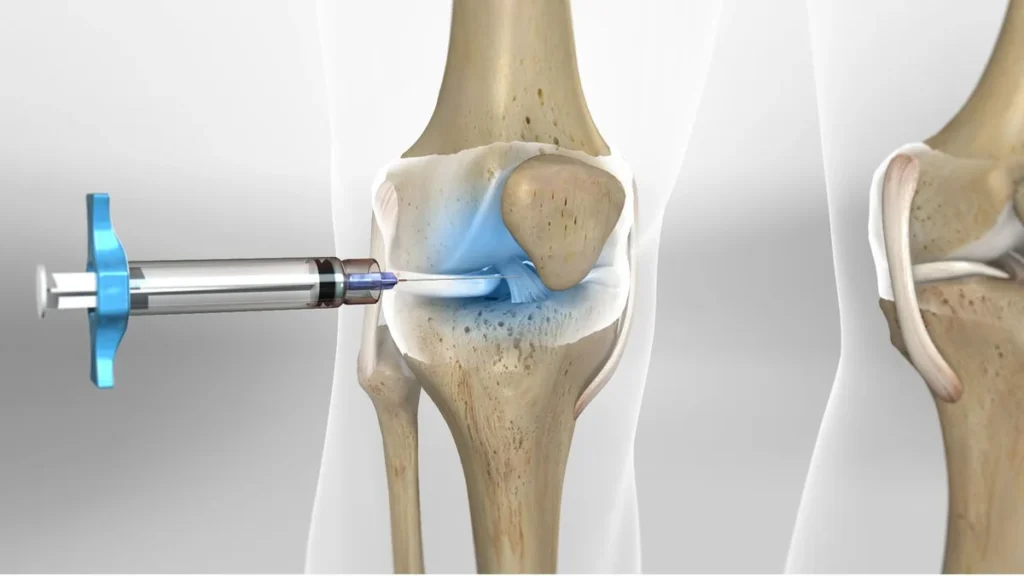
For patients with early stages of arthritis, it is recommended to first explore non-surgical and conservative approaches before deciding on joint replacement. These approaches include:
- Physiotherapy
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroid injections
The Process of Shoulder Joint Replacement Surgery
Shoulder joint replacement is performed by replacing the humeral head (joint ball) with a metal ball and the glenoid cavity (joint socket) with a soft plastic cup. Most often, this surgery uses a metal-on-plastic implant system. For some patients, such as those with severe humerus fractures, a “partial shoulder replacement” (hemiarthroplasty) is sometimes recommended, in which only the ball component is replaced.
Types of Anesthesia in Shoulder Joint Replacement Surgery
During total shoulder joint replacement surgery, the patient may receive regional anesthesia with an interscalene block, general anesthesia, or a combination of both. During surgery, the patient is usually positioned sitting up and may receive mild or complete sedation.
Stages of Traditional Shoulder Joint Replacement Surgery
Traditional shoulder joint replacement surgery consists of several key stages:
- The surgeon separates the deltoid and pectoral muscles to access the shoulder, especially in an area that is mostly nerve-free to prevent nerve damage.
- The shoulder is opened by cutting one of the front rotator cuff muscles, allowing the surgeon to view and manipulate the arthritic parts of the ball and socket.
- The arthritic joint parts are removed.
- The implant socket, ball, and stem components are installed.
- The cut in the rotator cuff muscle is closed and sutured.
- The external skin incision is cleaned and sutured, and a dressing is applied.
Reverse Shoulder Joint Replacement
Reverse shoulder joint replacement is a different procedure where the positions of the ball and socket are reversed. A metal ball implant is placed in the natural socket location, and a plastic socket implant is placed on the top of the humerus.
This reverse design, due to greater stability, is suitable for cases where tendons are damaged or non-functional. Movement in this method is controlled by the deltoid muscle, ideal for patients with shoulder arthritis and severe rotator cuff tears.
In a healthy person, the shoulder ball sits against the socket, but in the reverse replacement design, due to tendon damage or insufficient function, this ratio is reversed. This method helps patients who lack sufficient soft tissue to support stability and movement.
Types of Shoulder Joint Replacement Implants
Shoulder joint replacement systems consist of common main components: a metal ball facing a plastic (polyethylene) socket. However, their designs vary.
Anatomic Shoulder Replacement
In traditional shoulder replacement, the polyethylene socket is often cemented to the surrounding bone, at least in part. The prosthetic ball has a stem that is usually inserted into the humerus without the need for cement. The stem’s design promotes bone integration, where the patient’s natural bone grows into the prosthetic material.
Reverse Shoulder Replacement
In reverse shoulder joint replacement, the components are metal and plastic, but their positions are reversed. The metal ball is attached to the patient’s existing socket, and a new plastic socket is attached to the upper humerus. The stem is designed to be cementless and prevents bone from growing into the prosthesis.
Risks and Complications of Shoulder Joint Replacement
Complications in shoulder joint replacement surgery are rare but can include:
- Instability (dislocation of the ball from the socket)
- Infection
- Nerve damage
- Glenoid wear
- Stiffness (usually resulting from incomplete rehabilitation)
Recovery Time After Shoulder Joint Replacement Surgery
Generally, the recovery process after shoulder joint replacement surgery may take eight weeks or more. Several months may be needed before undertaking heavy physical work or intense strength exercises.
On the Day of Surgery
After surgery, the patient wakes up in the recovery room with their arm immobilized by their side in a movable canvas arm sling. Some temporary pain from the surgery is experienced, but arthritic pain significantly reduces.
The Day After Surgery
To confirm the correct position of the implant, an X-ray is taken. Physiotherapy begins the same day, focusing on improving mobility and reducing the sensation of grinding. The sling is used to support the repaired tendons but is removed for showering and rehabilitation exercises.
Full Recovery Timeline
- Six weeks: Light activity with the arm.
- Eight weeks or more: Active use of the arm and shoulder without restriction.
- Three months: Semi-normal range of motion and some weakness.
- Six months: Most patients are pain-free, with nearly two-thirds of the normal range of motion and strength.
- One year: Approximately 95% of patients are pain-free, with occasional pain under specific conditions.
Returning to Work
Returning to work depends on the patient’s progress:
- Two to three weeks: Return to desk jobs.
- Four months or more: For heavier physical jobs, depending on the condition of muscles and tendons before surgery.
In all cases, appropriate and extensive rehabilitation is vital to achieve the maximum benefits of shoulder joint replacement surgery.
Cost of Shoulder Joint Replacement
A primary concern for patients considering shoulder joint replacement is the cost and price of the surgery. A fixed cost determination is not feasible, as surgery costs vary for each individual and are influenced by several factors, including:
- Surgeon’s fees: Costs related to surgical services.
- Brand of materials and prostheses used: Choice of type and quality of prosthesis and materials used in surgery.
- Duration of hospital stay: Costs associated with staying in the hospital.
- Patient’s insurance type: Insurance coverage and the extent of insurance contribution to costs.

To make an appointment or get an online consultation with Dr. Nader Motallebi Zadeh, Limb lengthening surgeon, proceed here.