Diagnosing bone fractures can sometimes be very clear and straightforward. Often, there is no need for a doctor to diagnose whether a limb has been fractured, as individuals can recognize the fracture themselves. However, sometimes diagnosing a fracture is not simple.
Guidelines for Diagnosing Bone Fractures
To diagnose a bone fracture, a doctor follows a systematic and efficient method used for diagnosing all kinds of health problems and diseases.
This method involves the following steps:
- Review of History: The doctor talks to the patient and those around them, gathering important information about the incident and fracture. This includes details about the nature and moment of the accident.
- Physical Examination and Paraclinical Facilities: After reviewing the history, the doctor conducts a physical examination of the patient and, if necessary, uses paraclinical facilities like X-rays and other tests.
- Talking to the Patient and Relatives: Verbal communication with the patient and their relatives is very useful for gaining more precise information about the real conditions of the fracture.
During conversations with the patient and relatives, important questions must be asked, such as:
- Did the patient fall from a height or have an accident?
- If it was an accident, how did it happen and what type of vehicle was involved?
- If the patient fell from a height, what was the height and when did the incident occur?
Importance of Timely Hospital Visits in Fractures
The time of visiting the hospital in fracture cases is crucial. The later the hospital visit and treatment initiation, the more complications from the fracture can arise. In cases where the fracture is accompanied by a vascular complication, starting treatment as soon as possible leads to better results. It’s also important to know whether the fracture site was contaminated.
In open fractures, contamination can lead to wound infection and increase fracture complications. Questions about the patient’s pain, other symptoms, and under what conditions the pain worsens or lessens are examples of the queries posed.
Sometimes, this information alone is enough to diagnose a fracture or illness.
Are All Fractures Diagnosable by Asking the Patient?
Not all fractures are clearly diagnosable by questioning the patient. Some symptoms of fracture are obvious. For example, common signs that make people suspect a fracture include the inability to stand or walk after an incident or the inability to use a limb post-accident.
Deformity of the limb is also a clear sign of fracture. Limb bleeding that occurs a day or two after the incident can also indicate a fracture. All these signs are assessed through the patient’s history.
However, in many cases, the patient’s history alone is not sufficient. For instance, the mentioned symptoms could arise from fractures or from other injury-related or pathological issues. Another important point is that in the history of many fractures, there is a clear history of limb injury. However, stress fractures or pathological fractures may occur without an obvious injury history, or in cases of abuse where a child’s limb is fractured, the history of trauma might be intentionally concealed.
Key Considerations in the Patient History and Examination Process for Diagnosing Fractures
In the process of obtaining a patient’s history or medical background, the following aspects must be carefully considered. The goal of this stage of the examination is to gather information that not only assists in accurately diagnosing the patient’s issue but also ensures the provision of more appropriate treatment.
- Patient’s Age, Occupation, and Previous Medical History: Information related to the patient’s age, occupation, and history of previous illnesses can be useful in diagnosis and treatment. Medications the patient is currently taking also provide important information.
- Nature and Severity of Injury: The manner and cause of the injury to the limb should be examined. Was the injury due to a vehicle accident? Was the patient driving or walking? Was the injury a result of a fall from a height or during sports activity?
- Severity of Injury: The extent of the injury and impact should be determined. In case of an accident, the vehicle’s speed at the time of the incident is also crucial information. Did the accident occur on urban streets or rural roads, and was it at high speed? If the injury is due to a fall, the height of the fall should be specified.
- Patient’s Symptoms: The patient may report specific symptoms of the injury, which are important for diagnosis.
- Time Factor: The amount of time elapsed since the incident occurred also creates vital information. In some cases, like vascular injuries due to fractures or open fractures, the time between the occurrence of the injury and the start of treatment is extremely important.
- Environment of the Injury: The location and conditions in which the limb injury occurred should be identified. In open fractures, environmental contamination can increase the risk of infection.
- Examination of Vital Parts of the Patient: In this stage, the overall condition of the patient is assessed to identify any life-threatening injuries to other parts of the body that may be more critical than the fracture itself. For example, a blow causing an open fracture might have resulted in severe bleeding requiring immediate intervention.
Symptoms of Bone Fractures
Bone fracture symptoms are divided into two categories:
- First Category of Fracture Symptoms: This category includes symptoms that, if observed, might indicate a fracture. However, the presence of these symptoms alone does not confirm a fracture and must be verified by a doctor. These symptoms include:
- Deformation of the limb: Changes in the shape and structure of the bone or area, visible or detectable by touch.
- Local swelling in the limb: Swelling and puffiness in the injured area.
- Bleeding in the skin of the limb: Visible bleeding in the skin of the injured area.
- Impairment in limb function: Disability or difficulties in the functioning of the bone or limb.
- Pain upon touching the fracture site: Pain in the injured areas when touched.
- Pain during movement of the limb or the doctor’s attempt to flex the injured bone.
- Second Category of Fracture Symptoms: This category includes symptoms that strongly suggest the presence of a fracture. These symptoms include:
- Abnormal movement in the limb: Movement in areas where there are typically no joints, caused by the fractured bone.
- Crepitus sound during limb movement: The sound of grating that occurs due to the collision of broken bone pieces, referred to as “crepitus.”
It should be noted that each of these symptoms requires evaluation by a physician and diagnostic confirmation.
Examination Stages for Patients Suspected of Fractures
The examination of a patient for injuries due to trauma follows a logical procedure. The most important assessments in the medical examination are:
- Looking: A lot can be learned by looking at the limbs. Deformities, swelling, bleeding, abrasions, and wounds can be discovered by visual inspection.
- The presence of a wound on the fracture site does not necessarily indicate an open fracture. Often, skin wounds are not related to the fracture site and can be considered closed under certain conditions.
- Touching: By touching the limb, the degree of stiffness and swelling can be felt. Sometimes the sharp edge of the fracture site can be felt under the skin. Moving the limb might cause the fracture site to make noise, which is usually more felt than heard.
- Pressing on the fracture site usually increases pain severity. Moving the limb joints can also intensify the pain.
- Blood Supply Status of the Fractured Limb:
- Sometimes blood vessels at the fracture site are damaged. This vascular injury, which may occur in the artery, vein, or both, is caused by the same blow that caused the bone fracture.
- In some limb locations, blood vessels are so close to the bone that any displacement in the bones following a fracture can cause vascular damage. Sometimes the sharp ends of the broken pieces can cause vascular damage.
- These vascular injuries can manifest as either partial or complete tearing of the vessel. Sometimes, due to pressure on displaced bones or a hematoma (accumulation of blood in part of the body tissue) caused by the fracture, blood enters from outside and closes the vessel. Sometimes, due to a blow to the vessel, a clot forms inside, closing the vessel.
- Rarely, a blow might cause the vessel wall to bleed, and this bleeding can lead to the closing of the blood flow pathway in the vessel. Any of these events can lead to reduced blood supply to the part of the limb located beyond the fracture site.
A part of the medical examination includes assessing the blood supply status of the fractured limb. This examination should not only be done immediately after the fracture but also be regularly repeated during the first 48 hours afterward.
Even if the fracture has been treated, such as being put in a cast or undergoing surgery, the vascular status of the limb should be regularly evaluated. The reason for this repetition is that the patient’s vascular status is unstable in the first 48 hours.
It is possible that the patient’s vascular status may appear normal in the initial examination but gradually becomes problematic. Therefore, it is very important that the blood supply to the patient’s limb is frequently assessed.
Severe pain in the hand or significant swelling in the fingers after casting the upper limb can be a sign of poor blood supply following a fracture or even treatment and should be taken seriously.
Examination of the Vascular Status of a Limb
In the examination of the vascular status of a limb, the following points are taken into consideration:
- Color: Changes in the color of the limb, such as paleness or bruising, are significant and can indicate problems with the limb’s vascular system.
- Warmth: If the limb is cold, it may be a sign of insufficient blood supply.
- Pulse: Pulse is a good indicator for assessing the vascular status of a limb. In vascular problems, the strength of the pulse may decrease or may not be felt at all.
- In the upper limbs, radial and ulnar pulses at the wrist, and arterial pulses at the front of the elbow and under the armpit are examined. In the lower limbs, femoral pulse in the groin, popliteal pulse behind the knee, and anterior and posterior tibial pulses at the ankle are assessed.
- Capillary Return: When the tip of a finger or nail is pressed, the pressed area and its surroundings turn white. This color change is natural, as the reddish background in skin color is due to the presence of blood in the capillaries. When the skin is pressed, the blood is drained from the capillaries, changing its color to white. Upon releasing the pressure, blood immediately returns to the capillaries, and the color returns to its original state. This phenomenon is called “capillary refill.”
- Sometimes, when pressure is released from the skin, the color does not return quickly to its original state, and this return of color happens slowly. The cause of this delay is usually a disturbance in the blood flow of the limb. This method can be used to examine the vascular status of a limb.
- Changes in Sensation and Movement: When the blood supply to a limb is compromised, the nerves in that limb also suffer from reduced blood flow, causing functional disturbances. One of the signs of this functional disturbance is a decrease in tactile sensation in the skin.
- Decreased Tactile Sensation: If there is no direct nerve damage in a limb, decreased sensation can be a sign of vascular problems. When decreased sensation is due to direct nerve damage, usually one nerve in the limb is affected. However, in cases where the decrease is due to vascular issues, all nerves in the limb are affected.
- Examination of Motor Nerves: Although vascular problems in a limb may affect motor nerves, examining these nerves cannot help in identifying vascular issues. This is because examining a motor nerve actually involves examining the muscle that is stimulated and moved by that nerve.
- Doppler Ultrasound and Angiography: If examinations cannot determine the vascular status of a limb, methods such as Doppler ultrasound or angiography are used for a more detailed examination of the vessels.
- Additional Examinations After Fracture Diagnosis: After a doctor diagnoses a fracture, additional examinations are performed to determine whether the fracture is open and whether there is a wound on the skin that leads to the fracture site. Additionally, it is assessed whether the blood supply to the fractured limb is appropriate or has been disrupted due to the fracture. The nerve status of the fractured limb is also checked to see if it is appropriate or has been impaired due to the fracture. Furthermore, it is examined whether there is damage to the internal organs following the impact.
The answers to these questions are very important. For example, if the fracture is open or if the limb has suffered vascular damage following the fracture, the patient must undergo immediate surgery. Although identifying nerve damage in a fractured limb may not significantly alter the treatment approach, it must be diagnosed before starting treatment, not after. Otherwise, the patient may feel that the nerve problem in their limb was caused by the medical treatment.
Is It Possible for a Fracture to Remain Hidden and Undiagnosed?
Sometimes after a fracture occurs, it is possible for a patient to continue performing daily activities with the injured limb. In such cases, both the patient and even the doctor may think that no fracture has occurred. The following types of fractures fall into the category of hidden fractures:
- Impacted Fractures: These fractures usually occur in the upper parts of the humerus, such as the neck of the humerus, the lower parts of the radius just above the wrist, and also in the neck of the femur.
- Stress Fractures (Fatigue Fractures): These types of fractures typically occur in the second and third metatarsals and the shaft of the tibia.
- Carpal Bone Fractures: Among these, the fracture of the scaphoid bone is the most significant.
- Rib Fractures: Although these fractures are painful and may cause restricted breathing, they often do not receive sufficient attention and remain undiagnosed.
- Greenstick Fractures: These types of fractures are more commonly seen in the forearms of children.
Paraclinical Examination and Imaging for Fracture Diagnosis
After interviewing the patient and obtaining information from their acquaintances, the doctor utilizes paraclinical methods for the final diagnosis of a fracture, with imaging being the most important of these methods.
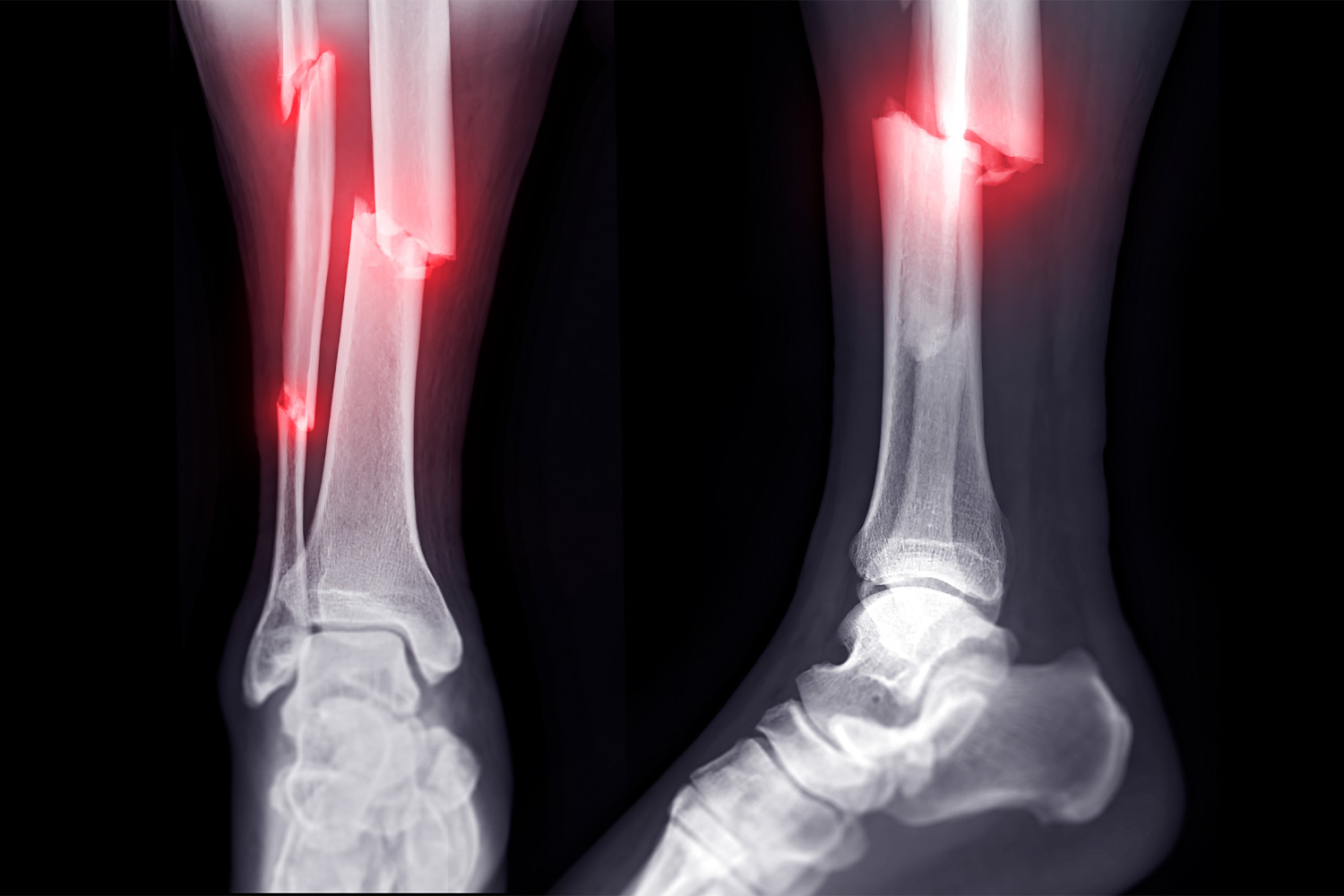
In the case of imaging a broken bone, the most important method is radiography or plain X-ray imaging. When there is suspicion of a fracture, radiographic imaging of the limb is essential.
Although in many cases there may not be a fracture and the radiographic result may be negative, failing to diagnose a fracture due to not performing radiography can have serious consequences. Therefore, we prefer to perform this procedure even if it appears to be repetitive.
How Radiography of a Fracture is Performed
The usual method for imaging an injured limb is taking two X-rays of it. First, an X-ray is directed from the front onto the limb and its image is captured on film, then the ray is directed again from the side of the limb.
The first image or film is known as the “antero-posterior” or “AP” view, and the second image is called the “lateral” view.
Producing a quality radiographic film is the art of the radiology technician. The amount and dose of X-rays applied to the limb must be carefully regulated. Any increase or decrease in this dose might result in a blurred image.
In the radiographic film, the entire length of the bone suspected to be fractured should be visible. Ideally, both the joint above and the joint below the bone suspected of having the fracture should be visible in the radiographic image.
The patient must keep their limb still during the imaging to ensure a clear picture is obtained. Also, all metal objects like rings or watches should be removed from the limb so that they do not obscure the image of the bone.
Diagnosing a bone fracture with radiography is not always simple. Sometimes, to examine the bone more accurately, radiographic images from different angles are needed. These images may be taken at oblique angles to the limb and are used to see finer details.
In some cases, the displacement of the broken pieces might be so minimal that it is not visible in the radiographic image. In these situations, if a radiographic image is taken again two weeks after the injury, the fracture line might become visible. This situation is particularly seen in fractures of the scaphoid bone.
Sometimes, diagnosing a fracture becomes very difficult. For example, in the radiographic image of a child’s elbow, many lines similar to fracture lines are seen and can be mistaken. In these cases, the doctor may take a radiographic image of both elbows and compare them to distinguish which lines are normal and which are abnormal.
An important point is that a bad radiographic film is much worse than not having a radiographic film at all. A poor-quality radiograph not only might fail to show the fracture but also can give the doctor and the patient a false sense of assurance that everything is fine and there is no problem.
In a radiographic image, the doctor pays attention to the following points:
- Type of Fracture: The doctor carefully examines the radiographic image to determine whether the fracture is a common fracture, a stress fracture, or a pathological fracture.
- Displacement of Fracture Pieces: If the fracture pieces have been displaced, the doctor tries to determine in which direction they have moved.
- Age of Fracture: The doctor assesses whether the fracture is recent or has been present for some time.
- Damage to Other Bones and Nearby Joints: The doctor in the radiographic image tries to thoroughly examine all the joints around the bone suspected of being fractured.
Important Points in the Preparation and Review of Radiological Images:
- Examination of Joints: In the examination of any bone, all joints surrounding that bone should be visible in the radiographic image. For example, in a radiographic image of the forearm area, the knee and ankle joints should also be visible in the image.
- Images of Important Areas: In cases where the patient is uncooperative in providing a history (such as an unconscious patient), radiographic images of the pelvis, neck, and chest should also be taken. Many injuries in these areas may not show specific symptoms during the examination and could remain undiagnosed and hidden without radiography.
- Supplementary Imaging: If a fracture of one calcaneus (heel bone) is seen in the radiographic image, images should also be taken of the other calcaneus and the vertebral column, as the likelihood of fractures in these areas is high.
- Imaging in Special Cases: In elderly individuals who experience pelvic pain after a fall, radiographic imaging of the pelvis is very important for detecting fractures of the femoral neck and pubic area. Many of these fractures initially have minimal displacement and can be very difficult to diagnose.
- Shoulder Fractures: In elderly individuals who experience shoulder pain after an injury, careful attention should be paid to fractures of the humeral neck and posterior dislocations of the shoulder joint. Sometimes the diagnosis of these injuries can be very challenging.
Other Methods in Bone Fracture Diagnosis
In most trauma patients, besides simple radiography, there is usually no need to use other imaging methods. However, in special cases, additional methods may be required to obtain supplementary information, including:
- Radioisotope Scanning:
- In radioisotope scanning, a radioactive substance, usually technetium diphosphonate 99, is injected into the patient. If there is a fracture, this substance is absorbed more in the fractured area than in other regions. Using special cameras, an image of the patient is taken and gamma rays from the radioactive material are recorded on the film.
- Areas that absorb more radioactive material emit more radiation and are clearly visible in the image. This method is usually used in cases where the presence of a fracture is suspected, such as the possibility of a scaphoid fracture or a stress fracture.
- In cases where there is a suspicion of non-displaced fractures, vertebral column fractures, or multiple fractures in the limbs, the use of radioisotope scanning can be very helpful.
- CT Scan:
- CT scans are often used to examine the shape of fractures, especially in areas where the bone has a complex three-dimensional shape, such as the vertebral column and pelvic bone. Sometimes a fracture may not be visible in a simple radiograph but can be detected with a CT scan. For example, a sacrum fracture that is visible in a CT scan may not be visible in a simple radiograph.
- MRI:
- MRI is primarily used to visualize soft tissues or non-bone tissues. These tissues may be damaged during a fracture, and sometimes the importance of soft tissue damage may be significantly greater than the fracture itself. For instance, in vertebral column fractures, examining the health of the spinal cord is very important, and MRI can effectively show spinal nerve damage.
- MRI is also used to examine non-displaced fractures and lesions of ligaments, menisci, and intervertebral discs.
- Angiography:
- In cases where the treating physician suspects severe vascular injuries, the use of angiography can greatly aid in the definitive diagnosis of these injuries. In this method, a special chemical substance is injected into the patient’s blood, followed by imaging of the targeted area. This substance allows blood and consequently blood vessels to be seen in the radiological image.

To make an appointment or get an online consultation with Dr. Nader Motallebi Zadeh, Limb lengthening surgeon, proceed here.
Thank you for reading the article “Diagnosing bone fractures” If you have any questions about Diagnosing bone fractures, feel free to ask us.