In this article from the limb lengthening center of Iran, we delve into the important topic of shoulder dislocation. The shoulder joint is recognized as the most mobile joint in the body. Its ability to rotate in many directions, however, increases its likelihood of dislocation compared to other joints.
The shoulder joint is formed by the combination of two bones: the head of the humerus and a part of the shoulder blade known as the glenoid cavity. The stability of the shoulder joint is largely maintained by the tissues surrounding it, such as the joint capsule, ligaments, and adjacent muscles. These tissues keep the head of the humerus within the glenoid cavity. In the event of a dislocation, these tissues are damaged.

Shoulder dislocation occurs when the head of the humerus comes out of the glenoid cavity. This type of dislocation is more common among all types of joint dislocations in humans, although it occurs less frequently in children.
Types of Shoulder Dislocation
Anterior and Posterior Shoulder Dislocation
Shoulder dislocations are primarily categorized into two main types: anterior and posterior. Anterior dislocation occurs when the head of the humerus bone moves out of the glenoid cavity and shifts forward. In contrast, in a posterior dislocation, the head of the bone moves backward or behind the cavity. Anterior dislocations are significantly more common than posterior ones. These dislocations often result from falling on an outstretched hand or directly on the shoulder.
During a fall, a person instinctively extends their hand forward to protect their head, resulting in the palm being the first part to contact the ground. This impact, especially if the hand is turned outward, can lead to anterior shoulder dislocation. This type of dislocation is also common in sports such as wrestling.
In an anterior shoulder dislocation, the joint capsule usually tears at the front of the shoulder, allowing the head of the humerus to dislocate. In this scenario, the head of the bone moves below the coracoid process and is sometimes referred to as a subcoracoid, or Subcoracoid dislocation.
Posterior shoulder dislocation occurs when a direct impact is applied to the front of the shoulder, pushing the head of the humerus backward. This type of dislocation can also occur following an electric shock or seizure. In these cases, due to the extreme internal rotation of the humerus, the head of the bone shifts backward. It’s possible for both shoulder joints to dislocate in these situations.
Clinical Symptoms of Anterior Shoulder Dislocation
The primary clinical symptoms of anterior shoulder dislocation include:
- Severe Pain: The most prominent symptom is severe pain, to the extent that the patient supports the injured arm and elbow with their healthy hand, preventing any movement of the shoulder.
- Shoulder Contour Change: Normally, when viewed from the front, the shoulder’s edge appears round and convex. In dislocation cases, this convexity disappears, making the acromion process the most prominent part on the shoulder’s edge.
- Bone Protrusion: Sometimes, the protrusion of the humerus head can be felt under the coracoid process, though this may not be discernible in overweight individuals.
- Risk of Vascular and Nerve Damage: In anterior dislocations, there is a risk of damaging the surrounding vessels and nerves. The Axillary nerve is most likely to be affected, indicated by a reduced sensation on the outer side of the shoulder.
Clinical Symptoms of Posterior Shoulder Dislocation
Posterior shoulder dislocation often lacks prominent symptoms and doesn’t cause significant visual changes in the shoulder, making diagnosis challenging.
A key symptom of posterior dislocation is that the patient’s arm remains in an internally rotated position, and they are unable to rotate the arm outwardly. Normally, if your palm faces forward when standing, it indicates external rotation of the arm; if it faces backward, it indicates internal rotation.
Normally, the protrusion of the humerus head can be felt under the acromion process. However, in posterior shoulder dislocations, this protrusion is not palpable.
Radiographic Imaging of the Shoulder Joint
Challenges in Simple Radiography
In simple radiographic imaging of the shoulder joint, diagnosing a dislocation may not always be straightforward. To address this, doctors sometimes use specific imaging techniques.
One such technique, known as the Axillary view, requires the patient to extend their arm away from the body as much as possible. Then, the X-ray is directed from under the armpit towards the shoulder. In cases of dislocation, raising the arm may be difficult, necessitating radiographs in oblique directions.
Treatment of Anterior Shoulder Dislocation
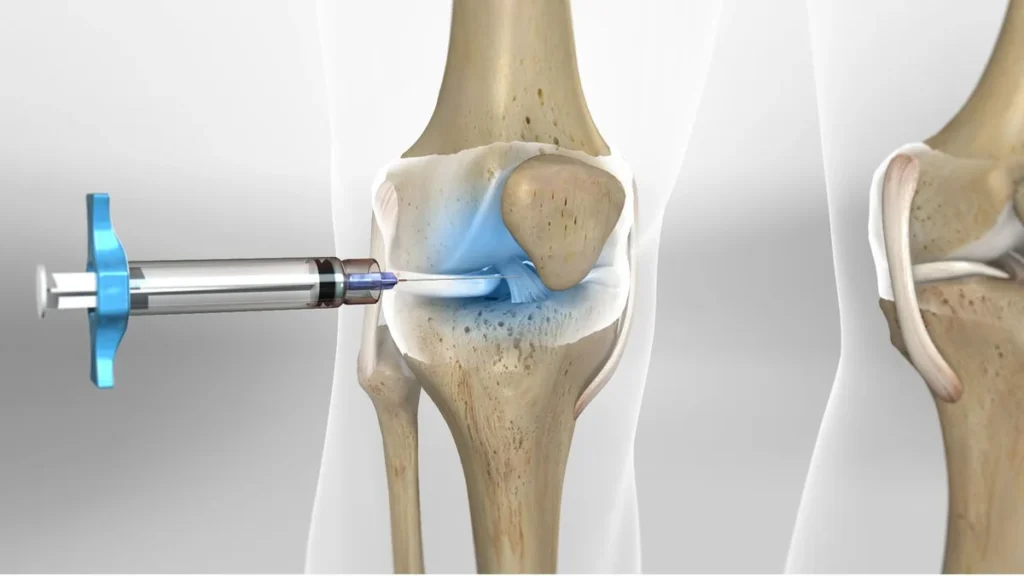
Reduction of the Dislocated Joint
In treating anterior shoulder dislocation, the first and most crucial step is the repositioning of the dislocated joint. The treating physician often performs this in an operating room using general anesthesia to reduce the patient’s pain. Sometimes, strong painkillers are used to help the patient tolerate the procedure. Various methods and maneuvers exist for repositioning the shoulder joint.
One common maneuver involves the patient lying supine with their arms extended. An assistant stands at the patient’s head, holding the ends of a sheet rolled into a tube and passed under the patient’s armpit. The physician stands beside the patient’s feet, grasping the patient’s wrist with both hands. The physician first moves the patient’s hand away from the body, then pulls it towards themselves, while the assistant also pulls the sheet in their direction. Sometimes, it may be necessary to apply pressure to the front of the humerus to move the head of the bone backward.
Kocher’s Method
Another method, known as Kocher’s technique, is executed as follows: The patient lies supine, and the physician stands beside the patient’s feet. The physician first bends the patient’s elbow at a 90-degree angle, gently moves the arm away from the body, and pulls it towards themselves. Then, the arm is rotated outward, brought close to the patient’s trunk, and the elbow is moved to the front of the chest. Finally, the arm is rotated inward so that the palm of the hand reaches the opposite side of the chest.
Radiographic Imaging and Treatment of Shoulder Dislocation
Complications in Kocher’s Method
While Kocher’s method is effective, it can have complications and, as such, is less frequently used.
Treatment of Posterior Shoulder Dislocation
For repositioning a posterior shoulder dislocation, a longitudinal traction method similar to that used in anterior dislocations is typically employed. The major difference lies in the application of pressure: it is applied from behind the humerus to push it forward. Post-reposition measures are similar to those for anterior dislocation.
Surgical Treatment for Shoulder Dislocation
Surgery may be necessary in specific and rare cases of shoulder dislocation:
- Dislocations that remain unreduced despite attempts at closed repositioning by a doctor.
- Dislocations are accompanied by displaced fractures in parts of the shoulder joint.
- Shoulder dislocations accompanied by a skin wound that has penetrated into the joint.
Immobilization of the Shoulder Joint After Repositioning
After repositioning the joint, the treating physician confirms the joint’s proper placement using radiography. Then, a special bandage called a Velpeau bandage is used to secure the patient’s hand to their neck and torso.
This bandage remains for about 2 to 3 weeks. Afterward, shoulder movements are initiated to prevent limited mobility. During this period, patients are advised to regularly move their hands, wrists, and elbows to prevent stiffness.
Immobilization after repositioning allows the tissues around the joint, torn during dislocation, to heal and reattach properly. If immobilization is not adequately observed, and the shoulder is moved prematurely, these tissues may not heal completely, leading to instability and laxity in the joint. This condition, known as recurrent shoulder dislocation, can make the joint prone to easy and repeated dislocations, even with minimal force.
Shoulder Joint Movement Post-Repositioning
On the other hand, keeping the joint immobile for an extended period can create problems, especially in older individuals who cannot tolerate several weeks of shoulder immobility. In these cases, prolonged immobility may quickly lead to joint stiffness, and the patient might lose the ability to raise their hand above their head after this period. Therefore, in older patients with shoulder dislocation, pendular shoulder movements are recommended a few days after repositioning and bandaging to prevent movement limitations.
After a certain period, under the supervision of a physician and physiotherapist, the patient performs specific exercises to strengthen the muscles around the shoulder.
In addition to acute dislocations typically seen in the shoulder joint, there are less common types of dislocations, such as recurrent, habitual, and old dislocations that have not been treated for a while, which can disrupt the functionality of the shoulder joint.
Recurrent Shoulder Dislocation
Sometimes, after repositioning a dislocated shoulder joint, it may dislocate again over time, potentially repeating frequently. As time passes, the frequency of dislocation increases, and the shoulder becomes prone to dislocating with less force. This dislocation may occur every time the patient raises their arm upwards and backward or rotates the shoulder outward. This condition, known as recurrent dislocation, is more common in young people, particularly during sports activities. Recurrent anterior dislocations are more common, while posterior recurrent dislocations are rare.
This issue is more frequent in individuals who did not adequately immobilize their shoulder after repositioning and returned to sports activities too soon. Each dislocation tears the joint capsule. If this tear does not heal properly due to insufficient immobilization after repositioning, the joint becomes unstable and can dislocate with the slightest impact.
Understanding Shoulder Dislocation and Its Complications
What is a Bankart Lesion?
The shoulder joint comprises the head of the humerus bone nestled in a shallow cavity called the glenoid fossa, a part of the shoulder blade. The joint capsule envelops the shoulder joint, encompassing both the humerus head and the glenoid fossa.
Surrounding the glenoid fossa is a cartilaginous ligamentous tissue known as the labrum, which deepens and extends the fossa. In severe shoulder dislocations, the labrum and the joint capsule may detach from the anterior edge of the glenoid. If this detachment does not properly reattach and heal post-repositioning, the shoulder becomes unstable at the front, leading to recurrent dislocations. This detachment of the labrum and joint capsule from the anterior glenoid rim is known as a Bankart lesion, indicative of recurrent shoulder dislocation.
Diagnosing Recurrent Shoulder Dislocation
The diagnosis of recurrent shoulder dislocation is mainly based on the patient’s reports of their previous experiences. Patients typically report dislocation occurrences in certain specific positions. Over time, they learn to reposition the dislocated joint independently.
A common situation where dislocation is likely is when the patient moves their arm upward and backward, rotating the shoulder outward. During this movement, patients often experience fear and apprehension of dislocation, known as the Apprehension test.
Radiographic images may show a lesion on a part of the humerus head, known as a Hill-Sachs lesion.
Treating Recurrent Shoulder Dislocation
The primary treatment for recurrent shoulder dislocation is surgery. The most common surgical procedure in these cases is the Bankart repair, where the detached joint capsule and labrum from the anterior edge of the glenoid are reattached to their original position. Nowadays, this surgery is mostly performed arthroscopically, a less invasive method.
Habitual or Voluntary Shoulder Dislocation
This less common type of dislocation involves the patient voluntarily dislocating and repositioning their joint. This condition is typically seen in individuals with familial joint capsule laxity.
Old Shoulder Dislocation
Sometimes patients are unaware of their shoulder dislocation, or repositioning does not occur for various reasons. This situation is known as an old dislocation. If less than six weeks have passed since the dislocation, the doctor cautiously attempts repositioning, mindful of the potential for humerus bone osteoporosis due to prolonged immobility, which could lead to fractures during repositioning.
If closed repositioning is unsuccessful or more than six weeks have passed since the dislocation, surgical repositioning is performed. In older individuals with high complication risks from joint repositioning, physiotherapy may be employed to improve shoulder movement.
Complications of Shoulder Dislocation
Treatment of shoulder dislocation typically involves closed repositioning and is often successful, allowing the patient to return to daily and sports activities. However, complications can arise, including:
- Axillary Nerve Damage: The axillary or circumflex nerve is often injured in shoulder dislocations. Symptoms include paralysis of the deltoid muscle and reduced sensation on the outer shoulder surface. The treating physician checks and records the nerve’s function before and after repositioning. In many cases, nerve function spontaneously improves over weeks to months. Severe damage may result in permanent paralysis and sensory loss.
- Damage to Other Shoulder Nerves: In rare cases, other shoulder nerves, particularly the posterior cord of the brachial plexus, may be injured.
Vascular and Fracture Complications in Shoulder Dislocation
Vascular Injury
In cases of anterior shoulder dislocation, the axillary artery can sometimes be damaged, particularly in older individuals who suffer from arterial stiffness or atherosclerosis. Additionally, in individuals with an old dislocation, the axillary artery may be injured during the repositioning of the joint.
Fractures Associated with Shoulder Dislocation
Occasionally, fractures in the neck of the humerus or in the greater tuberosity of the humerus occur alongside a shoulder dislocation. If the fracture of the greater tuberosity does not properly reposition, surgical intervention and fixation of the fragment with screws may be required. A fracture in the neck of the humerus, when accompanied by shoulder dislocation, usually requires surgery and is fixed with screws and plates.

To make an appointment or get an online consultation with Dr. Nader Motallebi Zadeh, Limb lengthening surgeon, proceed here.
Conclusion
Thank you for reading this article on shoulder dislocation. If you have any questions related to shoulder dislocation, feel free to ask in the comments section.